By Laurel White
The two researchers, with labs an ocean apart and seemingly little in common, were supposed to chat for just five minutes. But science and fate had much more in store.
As their conversation — set up by a colleague and mutual friend, a sort of academic blind date — moved from MRIs of human hearts and investigations of skeletal cells in mice to rare frozen tissue and even rarer expertise, those five minutes melted into hours and an opportunity for collaboration unfolded. Years later, the duo and their teams have made discoveries that could break new ground in how heart disease is treated in people with diabetes — and they’re just getting started.
Since that first meeting in 2016, Gary Diffee, professor in the School of Education’s Department of Kinesiology, and Chris Baldi, an associate professor of medicine at the University of Otago in Dunedin, New Zealand, have had quite the scientific adventure. They’ve mailed frozen heart tissue across an ocean (which they don’t particularly recommend), logged several flights over that same ocean (more highly recommended, even for a tall guy like Diffee), landed grants, published papers, and shaped the career of at least one young researcher.
“This is definitely the coolest thing I’ve done for a long time in my research,” Diffee says.
“I think it speaks to the benefit of really being open about science and not protective of your own idea,” Baldi says. “Gary convinced me to go in a different direction, and had I been precious about my own hypotheses, this never would have happened.”
Diffee and Baldi’s area of shared inquiry has to do with the unique complexities of heart disease for people with diabetes. According to the Centers for Disease Control and Prevention, people with diabetes are twice as likely to have heart disease than people without diabetes. The two health challenges often go hand-in-hand, but research has shown that many medications used to treat heart disease aren’t as effective for people living with diabetes.
“We know very little about what diabetes is doing to the heart — why it is damaging heart function, why it’s making treatment less effective,” Diffee explains.
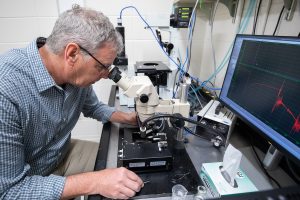
Baldi had been doing research on cardiac function and diabetes for a while before meeting Diffee. His research involved taking MRIs of hearts and using the images to examine how the organ reacted to things like exercise. Diffee suggested shifting the research toward a relatively rare technique he’d used for years in his own lab: examining the structure and function of single cells. Diffee argued examining the heart in such a granular way could reap big benefits for understanding how it works, or fails to work, under certain conditions.
“Gary is one of a small number of people in the world who do this type of research,” Baldi says.
The only problem: getting access to human heart tissue to run this sort of test isn’t simple.
“People are stingy giving up pieces of their heart if they’re not going in for heart surgery,” Diffee jokes.
Fortunately, Baldi had unique access to just what they needed: a bank of frozen heart tissue at the University of Otago. The tissue was collected from people who underwent heart surgery for different conditions and generously allowed small samples to be retained for research.
“It’s a perfect source of heart tissue for us to do single cardiac cell measurements,” Diffee says.

And so Diffee brought deep knowledge of a rare technique, and Baldi supplied an important research question and some hard-to-find materials — a tantalizing combination for any research scientist.
The first months of their collaboration were unique. Baldi mailed frozen heart tissue (pieces of left ventricle, to be precise) for Diffee to run tests on. The tissue included samples from people with diabetes, and people without. Their hypothesis: hearts of people with diabetes have decreased sensitivity to calcium, the stimulus that triggers contractions in heart cells. In other words, the presence of calcium, and adequate sensitivity to it, keeps the heart beating.
Baldi describes their first set of results as “jaw-dropping.”
“When we ran those statistics and they confirmed our hypothesis, we couldn’t believe it,” he says.
The pair’s first publication on the subject ran in the journal Cardiovascular Research in April 2018.
But it became apparent that the journey from New Zealand to Madison was too risky for such valuable tissue. The research arrangement as it was wouldn’t be sustainable.
“So we hit on this idea that I should just go down there and teach him how to do this,” Diffee recalls.
Baldi won a Catalyst Fund grant from the Royal Society of New Zealand to fund Diffee’s travel and the necessary equipment — a machine so delicate that it has to sit on an air cushion — and the duo were set up for a new phase of their transpacific collaboration. Later that year, Diffee made his first trip across the ocean and, soon after, was joined by another member of the UW–Madison science community: Angie Greenman.
Greenman, who earned her master’s degree in kinesiology at UW–Madison under Diffee’s leadership, moved to New Zealand to study for her PhD under Baldi’s direction. Because her master’s thesis focused on the effects of cancer on muscle, Greenman was well-versed in how to measure the amount of force produced by a skeletal muscle. In her PhD work in Baldi’s lab, she would help measure the amount of force produced by a single heart cell, which would help identify its calcium sensitivity.
“That’s really exciting to me because you can get to the nitty gritty,” Greenman says. “Once you go small, you can decipher the smaller details.”
Over the next few years (with a prolonged interruption due to COVID-19 pandemic travel restrictions), Diffee dropped in and out of Baldi’s lab. The team, which shifted to using more readily-available heart cells from diabetic rats for further research, published more papers on their findings in 2021 and 2022.
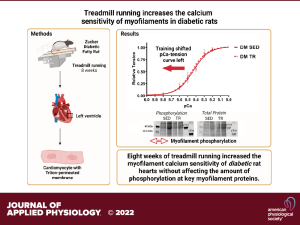
Those papers found different stages of diabetes affect cardiac calcium sensitivity differently and that exercise can increase the calcium sensitivity of heart cells in rats with diabetes.
Greenman says the knowledge that heart cells with reduced calcium sensitivity can respond well to exercise could offer hope to people with type 2 diabetes.
“The fact that you can have really well-controlled type 2 diabetes but it’s still a problem for your heart to do things like walk up the stairs or carry the groceries … it was really exciting to learn heart cells are malleable,” she says. “It’s really promising that you can have some control back in your life.”
The team has more papers in the works, and Baldi has several projects with colleagues at the University of Otago that have spun out of his research with Diffee. Diffee is also involved in one of those spin-off projects: a collaboration with University of Otago pharmacologists that has led to the early stages of a new drug that could be used to treat heart disease.
Treatments currently in use for acute heart failure, like adrenaline, work by increasing calcium movement in the heart. But a challenge with these drugs, Baldi explains, is that the movement of calcium in a cell requires a lot of oxygen — it’s asking an already overburdened organ to do something that’s pretty hard work.
“For a heart that’s failing, you’re asking it to do something too difficult,” he says. “It’s almost better to do nothing.”
This new drug under development, which has already received approval from the U.S. Food and Drug Administration for one condition, appears to offer a way to stimulate heartbeats without increasing calcium in the heart.
“If you apply the drug, the heart cell should have an increased calcium sensitivity,” Baldi explains.
He is cautiously optimistic about the drug, which could someday be a game-changer for heart disease treatment.

“There are no guarantees, and we may be wrong — you usually are, in science,” he says. “But what if we’re on to something?”
It’s a promising path forward, and one that wouldn’t have been possible if two researchers with seemingly little in common hadn’t sat down for a quick, five-minute chat seven years ago.
“I just think this is one of the best things about science,” Diffee says.